Why Stethoscover is Needed for Infection Control
85%
Average Stethoscope
Contamination Rate
75%
Clinicians not Disinfecting
in Between Patients
Stethoscope Contamination and Infection
Stethoscopes, used in 5.5 billion auscultations annually in the U.S., are crucial in healthcare but pose a significant infection risk. Known as a clinician's "third hand," they have an 85% contamination rate, contributing to the spread of hospital-acquired infections (HAIs). Despite this, 75% of clinicians do not disinfect stethoscopes between patient encounters. Research shows that stethoscopes may transmit similar amounts of infection as clinicians' hands and patients' skin. Click here to view our infographic on stethoscope contamination research Click here to view our infographic on stethoscope contamination research.
Ineffectiveness of Current Cleaning Methods
Current cleaning methods for stethoscopes are inadequate. Disinfection and sterilization, including alcohol-based swabs, fail to eliminate bacterial DNA. While investments are made in other infection control measures, stethoscopes are often overlooked. Prioritizing stethoscope hygiene is as vital as hand hygiene and using Personal Protective Equipment (PPE) like masks and gowns to prevent HAIs.
Ineffectiveness of Disposable Stethoscopes
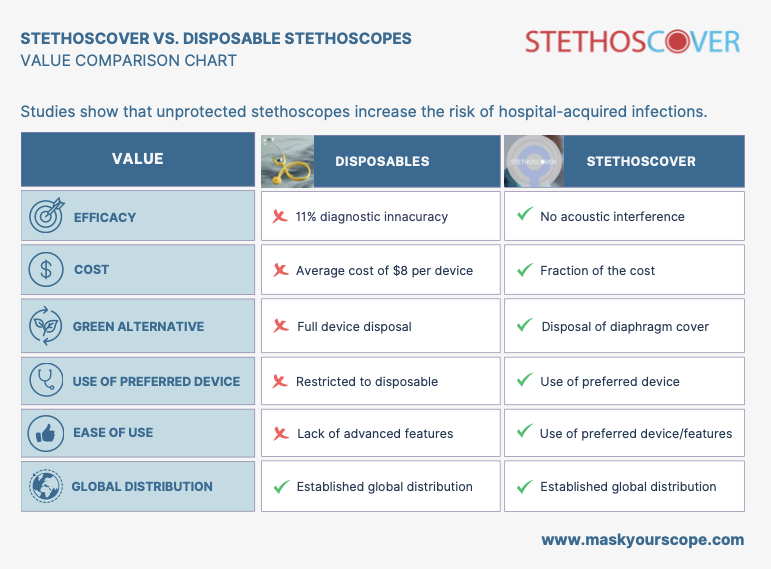
Disposable stethoscopes, also known as "single-patient stethoscopes," are recommended by the CDC for patients on contact precautions. However, they have upwards of 11% diagnostic inaccuracy due to acoustic interference, cost about $8 each, lack advanced features, generate waste, and still require cleaning. Click here to view our value comparison chart between Stethoscover and disposable stethoscopes.
Stethoscover: An Efficient and Effective Solution for Stethoscope Hygiene
Stethoscover acts as a barrier between the stethoscope and the patient, preventing nosocomial infections. Our touch-free, automated barrier application saves clinicians time, costs significantly less than disposable stethoscopes, and has zero acoustic interference. Integrating Stethoscover with hand washing and sanitation can significantly reduce HAIs and Multidrug-resistant Organisms (MDROs), ensuring stethoscopes are not disease vectors.
(1) https://apic.org/noncritical-is-critical/
(2) https://www.mayoclinicproceedings.org/article/S0025-6196(13)01084-7/fulltext
(3) https://www.cambridge.org/core/journals/infection-control-and-hospital-epidemiology/article/abs/predictors-of-heavy-stethoscope-contamination-following-a-physical-examination/2F0816C40D9FA733EC9F89654D3BF380
(4) https://www.google.com/url?q=https://www.infectiousdiseaseadvisor.com/news/stethoscope-cleaning-standards-may-not-eliminate-bacterial-contamination/&sa=D&source=docs&ust=1721989419435851&usg=AOvVaw1hc11LFHFxjVaN_YgCjDdv
